Psoriasis is a chronic autoimmune skin condition that affects millions of people worldwide, causing discomfort, emotional distress, and sometimes severe health complications. While it’s not life-threatening, recognizing its symptoms, identifying triggers, and seeking professional medical care are crucial for managing the condition effectively. If you notice any unusual skin changes, it’s important to consult a healthcare professional as soon as possible to prevent complications and ensure proper treatment.

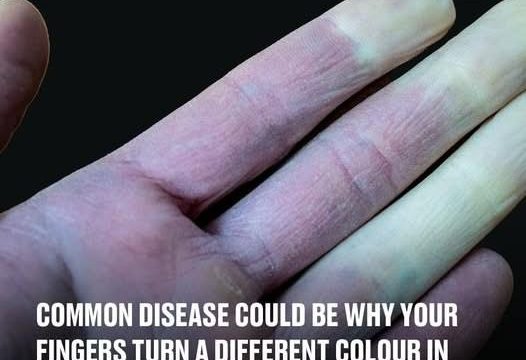
There are several types of psoriasis, each presenting distinct symptoms and affecting different parts of the body. Plaque Psoriasis is the most common type, characterized by red, raised patches of skin covered with silvery scales. These patches typically appear on the scalp, elbows, and knees and can cause itching, burning, and discomfort. Another type is Guttate Psoriasis, which manifests as small, pink, drop-shaped spots primarily on the trunk, arms, and legs. These lesions are usually thinner and smaller than those seen in plaque psoriasis. Pustular Psoriasis is more severe and primarily affects adults. It appears as red, inflamed skin accompanied by pus-filled blisters, often concentrated on the hands and feet but capable of spreading across the body. Inverse Psoriasis develops in areas with skin folds, such as under the breasts, around the groin, and in the armpits. It presents as smooth, shiny, red patches of irritated skin, often worsening with friction or sweating. The most severe form is Erythrodermic Psoriasis, a rare condition resembling an extreme sunburn. It causes widespread redness, peeling, severe pain, fever, and overall illness. This type of psoriasis is considered a medical emergency and requires immediate professional intervention.
Despite its sometimes alarming appearance, psoriasis is not contagious. You cannot catch or spread it through physical contact, sharing personal items, or being close to someone with the condition. Psoriasis is an autoimmune disease, not an infectious one, and stems from internal factors rather than external transmission.
The root cause of psoriasis lies in an overactive immune system. In individuals with psoriasis, T-cells, a type of white blood cell, mistakenly attack healthy skin cells. This triggers an overproduction of new skin cells, causing them to build up on the skin’s surface faster than they can be shed naturally. This buildup results in inflammation, itching, and the characteristic scaly patches. Genetics also play a significant role in psoriasis. Studies show that approximately 2–3% of psoriasis cases are hereditary, meaning if a close family member has psoriasis, your risk of developing it increases.
Certain factors can trigger or worsen psoriasis flare-ups. Excessive alcohol consumption is a known trigger, as it can weaken the immune system and interfere with treatment effectiveness. Similarly, certain medications, including lithium, antimalarial drugs, and specific blood pressure medications, have been linked to psoriasis flare-ups. Additionally, infections like strep throat can activate the immune system, leading to a sudden outbreak, particularly in guttate psoriasis.
Diagnosing psoriasis usually begins with a physical examination by a dermatologist. The doctor will carefully inspect affected skin areas, inquire about family and medical history, and evaluate your symptoms. In cases where the diagnosis is uncertain, a skin biopsy may be performed. A small sample of skin is analyzed under a microscope to confirm whether psoriasis is the cause of the skin changes.
While psoriasis cannot be cured, there are several effective treatment options that can manage symptoms and improve quality of life. Topical treatments are often the first approach, especially for mild to moderate cases. These treatments are applied directly to the skin and include corticosteroids to reduce inflammation, vitamin D analogues to slow down excessive skin cell production, retinoids to promote healthy skin renewal, and salicylic acid to help soften and remove thick scales. Additionally, regular use of moisturizers helps hydrate the skin and reduce irritation.
For moderate to severe cases, immunosuppressive medications may be prescribed. These drugs help modulate the immune system to prevent flare-ups and inflammation. Common options include methotrexate, which suppresses the immune response, and cyclosporine, which directly targets inflammation. In recent years, biologic drugs have emerged as a groundbreaking treatment for psoriasis. These medications target specific immune system pathways responsible for triggering psoriasis symptoms, providing significant relief for many patients. Another widely used treatment option is phototherapy, where controlled exposure to ultraviolet (UV) light helps reduce inflammation and slow skin cell turnover.
It’s important to recognize that psoriasis is a chronic but manageable condition. By identifying and avoiding triggers, adopting a healthy lifestyle, and following a tailored treatment plan, individuals can minimize flare-ups and improve their overall quality of life. While self-management plays a crucial role, regular consultations with a dermatologist are essential for monitoring symptoms, adjusting treatments, and preventing complications.
If you notice persistent red patches, scaly lesions, or unusual skin irritation that doesn’t improve with over-the-counter treatments, don’t hesitate to seek professional help. Early diagnosis and intervention can prevent the condition from worsening and help you regain control over your symptoms. Specialized medical facilities like Vinmec International General Hospital offer expert care, personalized treatment plans, and advanced therapies for psoriasis management.
In conclusion, psoriasis may be a long-term condition, but it doesn’t have to control your life. With the right approach, including medical care, proper treatment, and lifestyle adjustments, you can successfully manage symptoms and maintain a fulfilling and comfortable life. If you notice any concerning signs on your skin, don’t delay—schedule an appointment with a dermatologist today. Early action is the key to effective management and long-term relief.